Introduction to the toolkit
Welcome to Oregon’s Toolkit for Implementing Value-Based Payment (VBP)!
Oregon is one of the first states to develop a Compact between payers and providers to promote increasing use of advanced VBP models. This statewide VBP commitment is designed to achieve the “quadruple aim” of enhancing patient experience, improving population health, reducing costs, and improving the work life of health care providers. To achieve the triple aim, health care system transformation and payment reform must also focus on reducing health disparities and achieving health equity.
“Currently, the majority of health care is paid based on quantity, or fee-for-service (FFS). In contrast, VBP supports providers in delivering whole-person care and holds them accountable for improving quality, costs, patient experience, and — increasingly — equity.” Oregon VBP Compact Roadmap, 2022
Successful VBP arrangements require an active partnership as payers and provider entities shift from a volume to a value focus. This Toolkit will help clinicians, provider entities, and their payer partners prepare for new VBP arrangements, implement these arrangements, and overcome specific challenges to operating successfully within increasingly advanced VBP models.
You can use the Table of Contents to identify how to get started with new VBP models. Each action item in the VBP checklist is described in the relevant Toolkit section.
Section I: Understand VBP models
Section II: Get ready for VBP
Section III: Go live with VBP model(s)
Section IV: Understand VBP compact models
While the Toolkit presents information in a sequential order, the process of implementing a new or more advanced VBP approach is iterative. Therefore, you can jump from one section to another to focus on items that are of most interest, depending on where you are in your VBP journey.
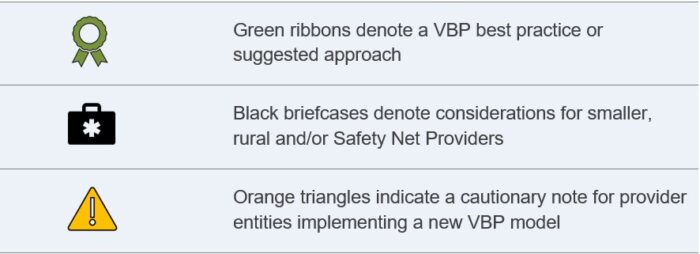
Throughout this document, the following icons highlight key actions and considerations for the reader.
While the primary audience for this Toolkit is expected to be provider entities and clinicians, important VBP considerations related to payers are highlighted in blue call-out boxes such as the following:
An ideal payer-provider VBP partnership includes communication, collaboration, data sharing, and technical assistance support, as well as prospectively defined value objectives, financial incentives, and appropriate protections.
Note: VBP models are also called alternative payment models (APMs). We use VBP in Oregon to emphasize the importance of value in the payment model.
VBP Toolkit Menu
- Understand VBP models
- Educate your team on VBP terms and models
- Assess internal interest and understanding of VBP
- Assess your readiness for a new or modified VBP model(s)
- Identify current data analytical capabilities and gaps
- Understand member attribution and assignment
- Understand your population and health disparities
- Understand types of financial risk in VBP models
- Get ready for VBP
- Go live with VBP model(s)
- Promote provider clinical transformation to foster VBP success
- Access technical assistance and peer learning
- Understand how quality is measured and used in different VBP models
- Maximize quality improvement – performance on measures
- Review results and make modifications
- Scale up current VBP contracts and engage additional payers
- Understand VBP compact models
- Primary care model
- Specialty care models (future content)
- Hospital care model (future content)
Health Equity: When all people can reach their full health potential and well-being and are not disadvantaged by their race, ethnicity, language, disability, geography, gender, gender identity, sexual orientation, social class, intersections among these communities or identities or other socially determined circumstances.
Payer: Any health insurance company, nonprofit hospital and medical service corporation, managed care organization, care coordination organization, and, to the extent permitted under federal law, any administrator of a health benefit plan offered by a public or a private entity.
Value-based payment (VBP) model: payment arrangement with provider entities that explicitly reward the provider entities’ performance on defined value objectives in the model. VBP models are designed to support providers in delivering whole-person care and holds them accountable for improving quality, costs, patient experience, and — increasingly — equity. VBP models are often categorized based on the LAN APM Framework.
Fee-for-Service: Providers receive a negotiated or payer-specified payment rate for every unit of service they deliver without regard to quality, outcomes or efficiency. [APM Framework Category 1]
Clinician: A doctor or other health care professional qualified in the clinical practice of medicine, psychiatry or psychology and having direct contact with, and responsibility for, patients.
Provider Entity: A legal entity that contracts with payers to provide health care to patients. Provide entities may include an individual physician(s) and/or other health care professional(s), a hospital or health system, a provider-sponsored organization, or any other kind of health care facility or organization responsible for direct care delivery to patients.